2024 Author: Josephine Shorter | [email protected]. Last modified: 2024-01-07 17:49
Causes, symptoms and treatment of lumbosacral radiculitis
Content:
- What is sciatica lumbar?
- Causes of occurrence
- Lumbar sciatica symptoms
- Treatment
What is sciatica lumbar?
Lumbosacral sciatica is a disease that affects the peripheral nervous system. With this pathology, compression and inflammation of the roots of the spinal nerves in the lumbosacral spine occurs.
This disease occurs quite often. According to statistics, about 10% of the adult population is subject to it to varying degrees. The risk group includes people of working age from 35 to 50 years. The main cause of the disease is degenerative-dystrophic changes in the spine (osteochondrosis).
Lumbosacral radiculitis is usually characterized by a chronic course, with periodic exacerbations of varying duration. The development of the disease is provoked by being and working in poor climatic conditions and significant physical exertion on the spine.
Causes of lumbosacral radiculitis

Lumbosacral sciatica is a complex of symptoms that occur when the roots of the spinal cord are irritated or compressed. It is not an independent disease, but a secondary pathological process.
It was previously thought that infection is the cause of sciatica. Currently, most experts are of the opinion that it is one of the consequences of the development of osteochondrosis (degenerative changes occurring in the intervertebral discs).
When the intervertebral discs of the spine receive insufficient nutrition, qualitative and structural changes of a non-inflammatory nature begin to occur in their tissues. The annulus fibrosus surrounding the nucleus pulposus of the disc dries out and becomes denser, and cracks form in it. As the degenerative process develops, the nucleus of the disc, together with the annulus fibrosus, protrudes into the intervertebral canal (disc protrusion), or the annulus fibrosus breaks and the nucleus comes out (herniated intervertebral disc).
At the same time, the height of the intervertebral discs decreases, the ligamentous apparatus is weakened. To compensate for excessive mobility and to prevent possible displacement of the vertebrae, bony protrusions, called osteophytes, grow at the edges of the vertebrae.
As a result, protruding or protruding discs, coupled with soft tissues, which are injured by osteophytes, put pressure on closely located nerve endings of the spinal cord, against the background of which a characteristic pain syndrome occurs. The progression of osteochondrosis can lead to complications such as stenosis (narrowing) of the spinal canal. This process can also capture foraminar channels. Bundles of nerve fibers leave the spinal canal through the foraminar openings between the vertebrae and go to the lower extremities and internal organs. Squeezing them causes the characteristic symptoms of sciatic nerve entrapment.
Additionally, the development of lumbosacral radiculitis can be triggered by:
- Spine injuries;
- Tumors of the peripheral nervous system;
- Other diseases such as arthritis or spondylolisthesis;
- Inflammatory process in the paravertebral soft tissues;
- Metabolic disorders (deposits of calcareous salts, provoking the formation of osteophytes);
- Autoimmune pathologies;
- Regular increased stress on the spine;
- Hypodynamia;
- Hereditary predisposition.
Another attack of sciatica can be caused by:
- Physical overvoltage;
- Hypothermia;
- Colds, flu;
- General intoxication;
- Abrupt or awkward movements of the lumbar spine.
Thus, the causes of lumbosacral radiculitis are polyetiological in nature.
Lumbar sciatica symptoms

Common symptoms of lumbosacral radiculitis include:
- Pain syndrome of varying intensity and localization, which is aggravated by sudden movements of the lower body, during falls, lifting weights and other physical exertion on the lower back;
- Increased pain when coughing, sneezing, tension of the abdominal muscles;
- Restriction of movement when the body bends to the sides, forward and backward;
- Movement disorders such as being unable to stand on your toes or bending your toes.
Depending on the level of the lesion, pain can be localized in different parts of the body: in the lumbar and gluteal regions, the back and front of the thigh, the muscles of the lower leg and calf. Also, pain syndrome can affect both one and both sides of the body. This is explained by the nature of the protrusion of the intervertebral discs (median or lateral).
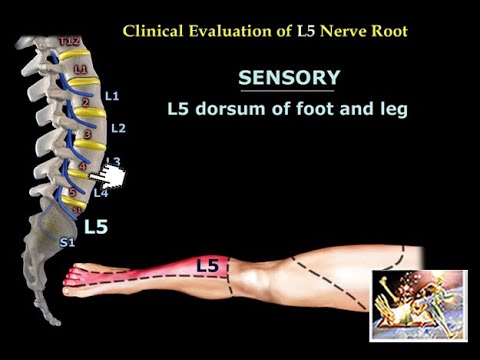
With the defeat of the nerve endings located under the I-II lumbar discs, there are lumbago in the lower back and buttock, pain passing along the back and lateral surfaces of the thigh. With damage to the nerves of the IV-V lumbar discs, the pain descends to the front of the lower leg, gastrocnemius muscle, external ankle and heel; there are violations of flexion of the foot and big toe.
The acute period of radiculitis lasts on average for 2-3 weeks. The following complex of specific symptoms is also used for its diagnosis:
- Ankylosing spondylitis symptom - there is a reflex flexion of the leg from the side of the lesion when moving from a supine position to a sitting position;
- Lasegue's symptom - pain in the lumbar, gluteal regions and the back of the leg increases sharply during the lifting of the straightened leg in the supine position;
- Dejerine's symptom - pain increases during coughing and sneezing;
- Bonnet's symptom - on the side of the lesion, the fold under the buttock is smoothed;
- Neri's symptom - pain in the lower body increases with a sharp tilt of the head forward.
For radiculitis caused by osteochondrosis, external changes in the body are also characteristic: straightening of the lumbar lordosis, increased kyphosis, scoliosis with bulging towards the lesion. With pathology of the disc between the V lumbar and I sacral vertebrae, the development of scoliosis with a curvature in the healthy side is possible.
Acute (influenza, malaria) or chronic (brucellosis) infections can cause infection of the nerve roots of the lumbosacral spine. The pain increases when the body is tilted forward and does not increase when the spine is loaded. Vegetative disorders are possible. In this case, with the extinction of the inflammatory process, the pain stops relatively quickly. There are no abnormalities on the X-rays.
Lumbosacral radiculitis treatment

Treatment of the disease is carried out depending on the causative factors and its stage (acute or chronic).
Conservative treatment is complex and includes:
- Bed rest (in the acute period);
- Wearing a corset to immobilize the spine;
- The use of drugs that relieve inflammation (in the form of injections, tablets, external agents);
- The use of muscle relaxants that eliminate muscle spasm in the lumbar region;
- Physiotherapy procedures providing anesthetic and prophylactic effect;
- Traction of the spinal column;
- Exercise therapy, aimed at strengthening the muscles and the formation of a muscle corset that supports the spine.
Medical treatment of lumbar sciatica
The most effective to this day are drugs from the group of non-steroidal anti-inflammatory drugs. They stop inflammation and relieve swelling. However, NSAIDs have a number of contraindications, have a negative effect on the gastrointestinal tract and are not recommended for long-term use.
On the subject: Injections from sciatica
With a sharp exacerbation, Diclofenac, Ibuprofen, Ortofen tablets are taken, in the future, after easing the pain, it is better to use ointments and creams that are applied to the places of pain localization. These include Finalgon, Apizartron, Diclofenac, Nise, Indomethacin. An ointment based on the snake venom Viprosal has proven itself well. Providing a local irritant effect, it improves blood circulation in the affected area.
Injections and blockages are prescribed for very severe pain. But they do not cure the disease, they only relieve the symptoms. Novocaine, Lidocaine, Trimecaine are used as anesthetics. Depending on the characteristics of the course of the disease, chondroprotectors or milgamma are placed.
Of the muscle relaxants, Mydocalm, Baksolan, Sirdalud are used. However, they also have many side effects and must be used once.
Physiotherapy for lumbar radiculitis

In the subacute stage, together with drug therapy, ultraviolet irradiation of the lower back and legs is performed along the affected nerve.
Electrophoresis with various drugs is often used: a solution of novocaine, a mixture of solutions of phenol, dicaine and adrenaline, with virapin ointment. Also, electrophoresis is done with an extract of therapeutic mud. With infectious radiculitis - with salicylates, copper solution, lithium.
In the acute stage with discogenic radiculitis, pulsed ultrasound therapy is prescribed, in which a mixture of analgesics can be used as a contact substance. As the symptoms subside, ultrasound is used in both pulsed and continuous modes. With the infectious nature of radiculitis, the combination of ultrasound with hydrogen sulfide and sodium chloride baths is effective.
Diadynamic currents, in which small electrodes are installed on the exit zones of the nerve roots and along the affected nerve, have shown themselves well.
With severe infectious lesions, physiotherapy is supplemented with injections of antibiotics or urotropin (intravenous).
With lumbar radiculitis caused by osteochondrosis, traction on an inclined plane is of great importance. It can be performed on a simple bed, the head of which is raised by 10-15 cm. The patient's body is fixed at the level of the head. Stretching can be short-term (2-3 times a day for 10 minutes) and long-term (up to 2 weeks), depending on individual tolerance.
On the subject: Home remedies for pain relief
Operative intervention
The indications for surgical intervention are (in combination):
- Pain syndrome that does not respond to conservative treatment for 3-4 months;
- Severe neurological symptoms;
- Signs of degenerative-dystrophic changes in the discs on the roentgenogram;
- Changes in the composition of the cerebrospinal fluid;
- Movement disorders;
- Dysfunction of the pelvic organs.
Exercises for radiculitis
Physiotherapy is an important component of therapy. It should be dealt with under the supervision of a doctor in the chronic stage of the disease and in subacute periods, to prevent relapse.
Before starting classes, it is necessary to assess the condition of the spine, check gait, identify the tolerance of traction and movements that increase pain. With discogenic radiculitis, back traction is an obligatory part of therapeutic exercises and is performed at the beginning and at the end of the complex.
The main exercises of the complex:
- Tensile;
- Relaxation;
- Respiratory;
- Passive and active exercises for the legs in the supine position.
During the introductory period, the main focus is on relaxation skills: the muscles of the arms, legs, trunk relax at rest and during elementary movements.
In the main period, stretching exercises are added. Each exercise should end with a relaxation of the muscles of the whole body. Hanging on hands on a horizontal bar or a gymnastic wall for 30-60 seconds are useful.
As the pain fades away, you can include strength exercises in classes (with objects or when your own body weight plays the role of burdening).
Corrective exercises to correct posture can be done only after the complete cessation of the pain syndrome.
A small complex for classes can be viewed in the following video:

Author of the article: Sokov Andrey Vladimirovich | Neurologist
Education: In 2005 completed an internship at the IM Sechenov First Moscow State Medical University and received a diploma in Neurology. In 2009, completed postgraduate studies in the specialty "Nervous diseases".
Recommended:
Sciatica - Gymnastics For Sciatica

Gymnastics for sciaticaInflammation of the sciatic nerve is most often caused by compression. This inevitably leads to painful sensations. In most cases, the reason for this is deformity of the vertebrae of the lumbar spine or displacement of the discs
Lumbar Kyphosis - Symptoms And Treatment

Lumbar kyphosisLumbar kyphosis is a pathological posterior curvature of the spine in the region of the five largest vertebrae. Most often, the pathological process involves two upper vertebrae of the lumbar spine and two lower vertebrae of the thoracic spine
Radiculitis Of The Cervical Spine (cervical Sciatica)

Radiculitis of the cervical spine (cervical sciatica)Content:Symptoms of cervical sciaticaCauses of cervical sciaticaTypes of cervical sciaticaDiagnostics of the cervical sciaticaTreatment of cervical sciaticaRadiculitis of the cervical spine is an active inflammatory process in the nerve root, which leaves the spinal cord in the cervical spine
Sciatica - Radiculitis Treatment At Home At Home

Radiculitis treatment at homeContent:Treatment of sciatica with fir5 more remedies for sciaticaAnti-inflammatory drugsIn case of salt metabolism disordersTreatment of sciatica with saltBanks for sciaticaExercise for the treatment of sciaticaCopper belt for radiculitisMustard plasters with honey will warm up sciaticaOther folk methodsTreatment of sciatica with firOne of the great ways to help get rid of sciatica is taking baths based on a decoction of fir paw
Radiculitis - Treatment Of Sciatica With Folk Remedies And Methods

Treatment of sciatica with folk remediesContent:Garlic relieves sciatica painTreatment of sciatica with sheep woolThe best remedy for radiculitis is a bathRadiculitis treatment with wild garlic tinctureTreatment of sciatica with rosemary ointmentTreatment of sciatica with clayRadiculitis treatment with saberTincture for radiculitis with "Triple" cologneTreatment of sciatica with sageRadiculitis treatment with oil and radishGarlic relieves sciatica painOne wo