Thromboembolytic complications
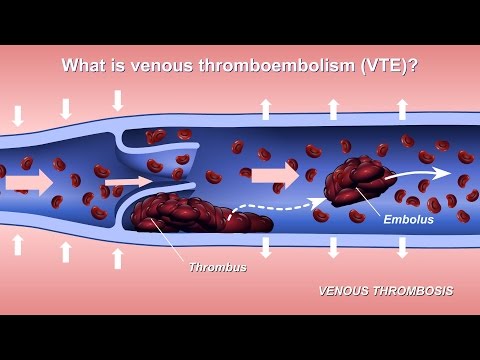
Thromboembolytic complications are an urgent problem in surgery. They cause severe health consequences and can lead to the death of the patient. As statistics show, in Russia alone, about 100,000 people die every year due to sudden pulmonary embolism. About 5% of patients die with the development of massive PE. In this case, a thrombus is detached, its disintegration into small particles, which clog small vessels, spreading through the body with the blood flow. Most blood clots form in the veins of the lower extremities, and from there they enter the vessels of the heart and lungs.
A blocked lung begins to suffer from oxygen starvation, as a result of which its tissues die off. The larger the blood clot, the more global the pathological changes. Extensive lung lesions lead to necrosis of large areas. This condition is called a pulmonary infarction. In the future, the patient develops respiratory and heart failure, which becomes the cause of death. Therefore, prevention of thromboembolytic complications in the postoperative period is an important task facing doctors.

It should be noted that thromboembolism can develop not only after surgery on the veins of the lower extremities. At risk are patients admitted to the urological, traumatological and gynecological departments of the hospital. That is, these are all patients for whom surgery is planned, or it has already been performed.
Other complications of the transferred venous thrombosis include thrombosis of the inferior vena cava, phlebothrombosis of the legs. They can also cause PE, but are life-threatening conditions in and of themselves.

Content:
- The causes of thromboembolism
- What are the risks of developing thromboembolytic complications?
- Symptoms of thromboembolytic complications
- How to recognize thromboembolytic complications
- Treatment of thromboembolytic complications
- How to avoid the development of thromboembolytic complications?
The causes of thromboembolism

Thromboembolytic complications develop both with impaired blood flow in the vessels of the lower extremities, and against the background of other predisposing factors.
There are three main reasons that lead to the formation of a blood clot. They are called the Virchow triad. So, thrombi are formed when the flow of blood through the veins slows down, when the integrity of the vascular wall is violated and when blood clotting is increased. All these three factors develop in patients in the early period after surgery.
The most dangerous surgical interventions in terms of the risk of thromboembolytic complications include:
- Operation on the abdominal organs. Moreover, even modern laparoscopy, carried out for therapeutic and diagnostic purposes, does not guarantee the absence of the risk of complications in the form of thromboembolism. They develop in 19% of the total number of operated patients.
- Operations on the internal genital organs located in the small pelvis. This can include uterine curettage and cesarean section. The risk of developing thromboembolism is equal to 11.2%.
- Urological operations, including prostate resection. The risks of complications reach 7.1%.
- Operations performed in neurosurgical departments. The risk of developing complications can be up to 24%.
- Removal of a malignant tumor from the body, regardless of its location. The risk rises to 30%.
- Operations for the received trauma of the lower extremities, as well as interventions carried out for prosthetics of the hip or knee joint. If the patient has been immobilized for a long time, then the likelihood of developing thromboembolytic complications increases to 84%.
Risk factors:
- Belonging to the female sex. It has been proven that blood clots are more often formed in women, which is largely due to hormonal fluctuations in their body.
- Senile age. As the body ages, the risk of blood clots forming in blood vessels increases.
- Sedentary lifestyle, sedentary work. These factors contribute to stagnation of blood in the veins.
- Varicose veins, which leads to disruption of their valve apparatus, to a slowdown in the rate of blood flow, to an increase in platelet aggregation.
- Taking hormonal contraceptives. These drugs affect the rheological properties of blood, thickening it.
- Hereditary predisposition to thrombophilia and increased blood clots.
What are the risks of developing thromboembolytic complications?
Depending on the nature and volume of the surgical intervention, the degree of risk of complications associated with thromboembolism varies:
- If the operation is not massive, for example, the patient undergoes laparoscopy or transurethral intervention on the prostate, then the risk of thromboembolytic complications does not exceed 0.2%. In this case, no more than 0.002% of all cases end in death. Such risks are considered low.
- Operations with a large volume of intervention, for example, resection of the gallbladder, removal of appendicitis, caesarean section, resection of the uterus, operations on the stomach and intestines, removal of prostate adenoma - all these procedures are associated with an average risk of thromboembolytic complications. They develop in about 5% of cases.
- Removal of a malignant tumor, surgery for fractures of the lower extremities, with joint replacement, as well as neurosurgical interventions carry a high risk of developing complications of thromboembolism. In patients, in 80% of cases, deep vein thrombosis of the leg is formed, in 40% of cases, thrombosis of the inferior vena cava, in 10% of cases, pulmonary embolism develops. In this case, some of the patients die.

Symptoms of thromboembolic complications

With deep vein thrombosis of the legs, a person experiences pain in the ankle and foot. The skin in this place changes its natural color, becomes purple or blue. The clot clogs the veins, which causes severe pain and insufficient blood supply to the tissues of the lower extremities. Therefore, if a patient who underwent surgery complains of pain in the lower extremities, they should not be ignored.
Pulmonary embolism manifests itself in different ways. If a small vessel was blocked, then the complication may remain undiagnosed until a certain point in time. As a result, the pulmonary and cardiac systems suffer. Often these patients develop chronic thromboembolic pulmonary hypertension.
It will be indicated by such health disorders as:
- Paroxysmal dry cough.
- Discharge during coughing of phlegm with blood.
- Pain in the chest.
- Suddenly developing shortness of breath, which may not be accompanied by physical activity.
- Feeling of lack of air.
- Episodes of loss of consciousness.
If the pulmonary embolism is massive, then the patient develops severe pain in the sternum, shortness of breath increases, and blood is present in the secretion separated from the lungs. The skin of the neck, face and earlobes becomes cyanotic. A horizontal line appears between the nipples, which also turns blue. Clinical death can develop rapidly, if there is no adequate therapy, then the patient dies. Sometimes death occurs very quickly: a person just gets up and falls. After a few minutes, his life ends.
How to recognize thromboembolytic complications
One of the informative methods for diagnosing venous thrombosis of the lower extremities is vascular ultrasound.
Pulmonary embolism with thrombotic masses can be detected by radiography, but if there are no global changes in the lung tissue, then the disease may remain undiagnosed. At the same time, anamnesis and assessment of the patient's condition provides assistance in determining thromboembolism.
Blood test for D-dimer, for its rheological properties (fibrin level, INR, APTT, PTT, PTI) - all these tests make it possible to clarify the diagnosis. Treatment is started immediately after the problem is discovered.
Treatment of thromboembolytic complications

If a patient with pulmonary embolism does not receive medical care, then his death occurs in 90% of cases. Therefore, therapy should be carried out as early as possible.
The doctor should direct efforts to dissolve the blood clot, as well as increase the fluidity of the blood. Therefore, the patient is shown intravenous administration of the following drugs:
- Low molecular weight heparins. For 5-7 days, the patient is administered Heparin at a dosage of 31-33,000 IU per day. Or replace Heparin with Enoxaparin at a dosage of 180 mg per day.
- Thrombolytic drugs: Streptokinase (250,000 IU in the first half hour, and then 100,000 IU during the first 24 hours) and Alteplase (100 mg in the first 24 hours).
For oral administration, warfarin 10 mg may be indicated for a week.
If necessary, a cava filter is installed in a patient with thrombosis. It is injected into the lumen of the inferior vena cava.
The operation for thromboembolytic complications is performed in the following cases:
- Recurrence of pulmonary embolism in the presence of sufficient anticoagulant treatment.
- Massive thrombosis of the inferior vena cava.
- Previously transferred or planned surgery in a patient with pulmonary embolism.
How to avoid the development of thromboembolytic complications?

In order to prevent the development of thromboembolytic complications, the following preventive measures are taken:
- If a person has undergone surgery, they should be raised as soon as possible.
- The patient should wear a compression garment that prevents blood from stagnating in the veins. If a person uses elastic socks, then the risk of thrombosis decreases to 8.6%, and if he wears stockings, then the probability of its formation decreases to 3.2%. If such underwear is used by a person with average and minimal risks of developing complications, then the probability of their occurrence becomes zero. Therefore, compression garments must be available for every patient who has undergone surgery.
- Intermittent pneumatic compression is used to improve blood flow through the veins of the lower extremities. For this, an air-pumping cuff is used, which is applied to the thigh and ankle under a pressure of 20 mm. rt. Art. and on the thigh under pressure of 35 mm. rt. Art.
- For prophylactic purposes, the patient is injected with Heparin even before the operation. The injection is performed subcutaneously at a dosage of 5000 units. After the surgery, a seven-day course of injections is shown at a dosage of 5000 IU, 3-4 times a day.
- Warfarin is prescribed to all patients who have no contraindications to its use. The dosage is 2.5 mg / day. The treatment lasts 30-45 days.

The author of the article: Volkov Dmitry Sergeevich | c. m. n. surgeon, phlebologist
Education: Moscow State University of Medicine and Dentistry (1996). In 2003 he received a diploma from the Educational and Scientific Medical Center of the Presidential Administration of the Russian Federation.