2024 Author: Josephine Shorter | [email protected]. Last modified: 2024-01-07 17:49
Acute renal failure: symptoms and treatment

Acute renal failure is a sudden, pronounced impairment, or complete cessation of kidney function. This pathological process is potentially reversible, although in the course of it all kidney functions suffer - excretory, filtration and secretory.
According to available statistics, about two hundred people develop acute renal failure out of every million people in Europe. More than 50% of cases of pathology are caused by operations on the heart or on large vessels, as well as multiple injuries. From 15 to 20% of cases of acute renal failure occur in obstetric practice. In addition, over the past 10 years, there has been an increase in the number of cases of acute renal dysfunction while taking medications. It is noteworthy that in African countries, renal failure develops mainly against the background of viral or parasitic infection. While in European countries, the cause is most often arterial hypertension and diabetes mellitus.
Content:
- The causes of kidney failure
- Stages and symptoms of kidney failure
- Complications of kidney failure
- Diagnosis of renal failure
- How is kidney failure treated?
- What kind of treatment can be arranged at home?
- What drugs are used to treat acute renal failure?
- Which doctor treats kidney failure?
The causes of kidney failure
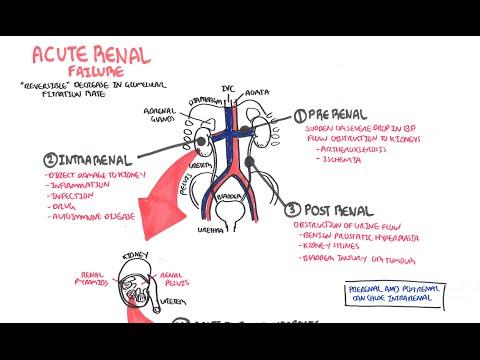
The causes of renal failure are multiple, but they are all combined into three large groups, which simultaneously represent the forms of the disease.
Causes of prerenal kidney failure (hemodynamic form):
- Decrease in cardiac output, which is observed in heart failure, arrhythmia, cardiogenic shock, pulmonary embolism, cardiac tamponade;
- A pronounced decrease in the level of extracellular fluid, which may be due to diarrhea, prolonged vomiting, severe blood loss, dehydration, burns, ascites against the background of cirrhosis;
- Intestinal obstruction, peritonitis, acute pancreatitis, as conditions leading to the sequestration of fluid in the tissues;
- Vasodilation of systemic genesis against the background of sepsis, anaphylaxis, endotoxic shock, or taking vasodilators.
Causes of renal renal failure (parenchymal form):
- Toxic effect on the parenchyma of the kidneys of poisons, fertilizers, cadmium, mercury, uranium, copper salts. Perhaps the development of a pathological condition against the background of bites of poisonous snakes and insects;
- Uncontrolled intake of drugs that have a toxic effect on the kidneys. Among these are sulfonamides and some other antibiotics, antineoplastic agents. If a person already has impaired renal function, then the introduction of contrast agents to perform an x-ray examination, as well as all of the above drugs, can cause the development of acute failure, even if the dosage is observed;
- An increase in the level of hemoglobin and myoglobin in the blood with a coma of alcoholic or narcotic origin, with inappropriate blood transfusion, with macrohemaglobinuria, against the background of prolonged compression of tissues;
- Inflammation of the kidneys, although rare, can still lead to the development of kidney failure. These are glomerulonephritis, tubulointerstitial nephritis;
-
Infectious diseases - hemorrhagic fever with severe renal syndrome, viral hepatitis, leptospirosis, HIV infection, etc.;
- Removal of one kidney or its injury.
Causes of postrenal kidney failure (obstructive form):
- Urolithiasis with obstruction of the urinary tract stones, which leads to a violation of the passage of urine;
- Tumor of the prostate gland, ureters, bladder;
- Dystrophic lesions of the retroperitoneal tissue;
- Urethritis, periurethritis;
- Kidney tuberculosis;
- Accidental ligation of the ureter during surgery.
Sometimes a combination of several factors causing renal failure is possible.
Stages and symptoms of kidney failure

The symptoms of kidney failure will vary depending on the stage of the disease:
- Symptoms of the initial stage of the disease. The patient's condition will be determined by the disease that provoked renal failure. Therefore, a person is not able to determine its manifestation on his own, the pathogenesis is veiled by the symptomatology of the etiological factor. Although circulatory collapse occurs, it is short-lived and therefore goes unnoticed. Symptoms of impaired renal function, such as loss of appetite, nausea and weakness, are attributed by the patient to an injury, poisoning or other condition that led to the manifestation of the process of renal failure.
-
Symptoms of the oligoanuric phase of the disease. The complete absence of excreted urine is rarely observed, but its volumes are significantly reduced (up to 500 ml or less per day).
In addition, violations such as:
- Severe proteinuria - high protein content is found in the urine;
- Azotemia - an increase in the content of nitrogenous metabolic products in the blood;
- Hyperphosphatemia - an increase in the level of phosphates in the blood;
- Metabolic acidosis with nausea and vomiting, drowsiness, increasing weakness, rapid breathing and shortness of breath;
- Arterial hypertension is diagnosed in 20-30% of patients;
- Hypernatremia - increased sodium content in the interstitial space;
- Hyperphosphatemia - an increase in the level of phosphate in the blood;
- Acute uremia provokes damage to the liver (with its increase in size) and other organs of the gastrointestinal tract. It is possible to develop gastrointestinal bleeding due to ulcers, which is found in 10-30% of cases.
Against the background of overhydration, pulmonary edema is possible, which is expressed in the occurrence of wet wheezing, the appearance of shortness of breath. In addition to the fact that the patient becomes inhibited, there is a threat of entering a coma.
Another common symptom of this stage of the disease is pericarditis and uremic gastroenterocolitis. These conditions are often complicated by bleeding.
Against the background of a weakening of the immune forces, an infection is possible. The development of sepsis, pancreatitis, stomatitis and pneumonia is not excluded. Acute infections greatly worsen the condition of patients.
This stage develops in the first three days after the body was affected by one or another etiological factor that led to renal failure. The oligoanuric stage lasts from 10 days to 2 weeks, however, it can shorten to several hours, or stretch for 2 months. If the oligoanuric stage lasts more than 4 weeks, it is necessary to exclude renal vasculitis, glomerulonephritis, necrosis of the renal cortex.
- Symptoms of the stage of recovery of diuresis. A striking symptom of this phase is polyuria, which develops against the background of the fact that the destroyed renal tubules have lost their ability to reabsorb. The daily urine output gradually increases and can range from 2 to 5 liters. The water and electrolyte balance gradually returns to normal. However, there is a danger of developing hypokalemia due to the leaching of potassium in the urine. This phase lasts an average of two weeks. If the patient receives inadequate therapy for the situation, then dehydration, hypophosphatemia, hypocalcemia may develop.
- Complete recovery stage symptoms. At this time, the kidney function is restored to its original level. This period can take from six months to a year. However, it is possible that acute renal failure will develop into chronic. This happens when most of the kidney tissue is affected.
Complications of kidney failure
Complications of renal failure depend on how severe the organ dysfunctions are, as well as on the presence of oliguria. It is against the background of bright oliguria that the level of glomerular filtration falls, which reduces the intake of electrolytes, nitrogen metabolism products and water. As a result, the blood composition suffers greatly.
- Disruptions in water-salt metabolism. The most dangerous in this regard is hyperkalemia, since against its background patients begin to complain of muscle weakness, sometimes tetraparesis and bradycardia form. The higher the concentration of potassium in the blood, the higher the risk of cardiac arrest.
- Blood composition disorders. Since the level of nitrogen in it rises, this becomes the cause of the rapid death of red blood cells. As a result, a complication such as normocytic normochromic anemia develops.
- Immunity dysfunctions. This leads to the fact that patients develop various infections, which occurs in 30-70% of cases. Complications in the form of immune disorders are very dangerous, since it is the joined infections that most often lead to death. The oral cavity suffers, postoperative wounds do not heal for a long time, the respiratory and urinary system may be damaged. Sepsis, as the most formidable complication of deficiency, is usually triggered by gram-negative and gram-positive bacteria.
- Disturbances from the nervous system are manifested in the fact that a person has confusion, lethargy, which is replaced by excitement. Space disorientation is possible. Neuropathy often develops in old age.
- From the side of the cardiovascular system, complications such as arrhythmia, congestive heart failure, arterial hypertension are possible.
- On the part of the digestive system, complications such as nausea, vomiting, abdominal pain, lack of appetite, bleeding against the background of gastroenterocolitis are possible.
Diagnosis of renal failure

Diagnosis of renal failure includes the delivery of a variety of tests, including:
- Blood to determine the level of potassium, nitrogenous compounds;
- Zimnitsky urine test;
- Biochemical blood test to determine the level of urea, electrolytes, creatine;
- Urine is also sent for general and bacteriological analysis.
Failure is detected by examining the bladder. There is no urine in it. It is important to distinguish between anuria and acute urinary retention, which can also accompany failure. With an overflow of an organ with urine, anuria does not develop.
As for instrumental examination methods, it is necessary to perform ultrasound of the bladder and kidneys to determine the form of insufficiency. It will be possible to judge the presence or absence of urinary tract obstruction.
Doppler ultrasonography of renal vessels is performed to assess blood flow in organs. A kidney biopsy is done to make a differential diagnosis.
A chest x-ray may be performed to rule out pulmonary renal syndrome and pulmonary edema. Chromocystoscopy is indicated if there is a suspicion that the orifice of the ureter is obstructed.
An electrocardiogram is taken for each patient with renal failure in order to detect arrhythmia in time.
How is acute kidney failure treated?
Treatment of renal failure is determined primarily by the stage at which the disease is, as well as by the factor that provoked the development of the pathological process. The success of therapy also depends on the patient's close interaction with doctors, nephrologists and urologists.
The primary goal is to eliminate the etiological factor that caused the failure of the kidneys. In parallel, measures are being taken to eliminate the existing shock, to normalize the work of the heart, and to replenish blood loss. It is important that the vessels are in good shape, and the blood flow in the kidneys is restored.
Detoxification measures should be carried out when the patient has been poisoned by salts of heavy metals, which led to the development of insufficiency. These are measures such as taking enterosorbents, gastric lavage, hemosorption.
To get rid of the patient from postrenal insufficiency, it is necessary to remove the obstruction of the urinary tract. For this, catheters can be installed in the ureters, nephrostomy and pyelostomy are performed.
So, the initial stage of insufficiency requires a decrease in the effect of nephrotoxins on the body, the elimination of circulatory disorders. If acute insufficiency has not yet manifested, but only threatens to develop, then it is possible for prophylactic purposes to intravenously administer the drug Mannitol, which helps to improve filtration and works as an osmotic diuretic. It makes no sense to apply it at the oliguric stage.
It is important to understand that therapy aimed at eliminating the cause that provoked the failure will be effective only if it is carried out at the initial stages of the development of pathology. In addition to therapeutic measures, quality care for the oral cavity, mucous membranes and skin is required. It is possible to prescribe antibiotics if the bacterial flora is isolated. However, these drugs are often prescribed to prevent the development of a bacterial infection. However, it is advisable to abandon Streptomycin, Neomycin and Monomycin, since they have increased nephrotoxicity.
With the oligoanuric form of the disease, the patient is prescribed hardware extracorporeal dialysis, as well as powerful detoxification therapy.
In order not to provoke hyperhydration, water intoxication, it is necessary to carefully monitor the volumes of fluid assigned to the patient in the oliguric and anuric periods.
As for the nutrition of patients, in the first three phases of the development of pathology, protein must be completely excluded from the diet. Eating sour cream, cream, syrups is possible. If dyspeptic disorders are persistent, then the patient is transferred to the parenteral route of nutrition.
To flush out nitrogenous toxins that provoke severe vomiting and nausea, it is necessary to carry out prolonged gastric lavage. Against the background of seizures, calcium salts are administered parenterally.
All forms of kidney failure require a person to be hospitalized. According to the indications, he is given hemodialysis. Sometimes it is performed before surgery - before nephrostomy or before pyelostomy. Surgical intervention is performed on the kidney that functions better. The evaluation criterion in this case is clinical signs. The pain will always be more intense where the kidney works best. After the anuria is eliminated, the patient is prescribed drugs aimed at normalizing renal blood flow and increasing the rheological properties of blood.
It should be borne in mind that hemodialysis can save the life of even the most severe patients, therefore, it should not be abandoned. It is effective even in the arena forms of pathology, when the patient's condition is very serious. After hemodialysis, it becomes possible to perform kidney transplantation.
Puncture nephrostomy is performed in the presence of a malignant tumor in the pelvic region or in the retroperitoneal space, in the event that the patient has obstruction of the ureters.
Unithiol is prescribed for the development of a deficiency formed during mercury poisoning.
Osmotic diuretics, a combination of Dopamine with Furosemide, help to normalize the patient's condition. The combination of two methods - hemodialysis and hemosorption of blood by the extrarenal method - makes it possible to correct the salt and water balance.
Indications for hemodialysis artificially by the kidney:
- Lack of effect from conservative treatment.
- The indicator of creatine in the blood is more than 114 mmol / l.
- Residual nitrogen exceeds 113 mmol / L.
- urea is above 49 mmol / l.
It is impossible to perform dialysis with sepsis, against the background of myocardial infarction, with bleeding of the gastrointestinal tract, against the background of hepatic and heart failure, with thromboembolism during an exacerbation.
Visiting resorts for the prevention of pathology is advisable no earlier than six months after the patient was discharged from the hospital.
As for the prognosis for recovery, it completely depends on the severity of the course of the disease, on the age of the patient and on how successfully the cause that led to the acute disruption of the kidneys is treatable. With adequate therapy, full recovery is observed in 35-40% of cases, partial - in 10-15%. Up to 3% of patients will need constant hemodialysis. The renal form of the disease is considered especially unfavorable in this regard. After it, more than 40% of patients are transferred to permanent hemodialysis.
The death of patients occurs due to uremic coma, from sepsis and hemodynamic disorders. Oliguria worsens the prognosis. The uncomplicated course of pathology, which developed initially, makes it possible to predict a complete recovery in 90% of cases. However, a timely visit to a doctor is an important condition.
What kind of treatment can be arranged at home?
Regarding what kind of treatment for acute renal failure can be carried out at home, the answer can be unambiguous - you need to immediately call an ambulance. Acute renal failure is a serious condition that poses a threat to the patient's life and requires emergency hospitalization. It will not be possible to cure a person at home.
The later qualified assistance is provided, the worse the prognosis. In addition, with early treatment, there is a chance that the person will recover in the next few years.
What drugs are used to treat acute renal failure?

- To relieve the symptoms of intoxication, the introduction of a solution of Sodium bicarbonate (2-3%) + insulin and glucose is shown.
- To prevent the development of pathology, Mannitol (20%) is injected in a volume of 300 ml. The drug should be used as early as possible.
- As an osmotic diuretic, glucose solution (10-20%) + insulin acts. It is administered intravenously in the first hours of the manifestation of renal failure in a volume of 0.5 liters.
- Dopamine + Furosemide for 6-24 hours. Dose of Dopamine from 3 to 5 mcg per kg per minute, Furosemide from 30 to 50 mcg per kg per hour.
- Venoruton by injection or orally three times every 24 hours.
- Intramuscularly, or under the skin of Unitiol, if the pathology proceeds against the background of mercury poisoning. The dose is 1 ml for every 10 kg of the patient's body weight.
- Trental intravenously or orally. 100 mg is injected intravenously, 1-2 tablets are taken orally three times every 24 hours.
- Intravenous Furosemide 200 mg + Mannitol.
Which doctor treats kidney failure?
A urologist and a nephrologist treat renal failure, however, if you suspect a manifestation of this condition, you need to call an ambulance, and not wait for the next appointment.

Author of the article: Lebedev Andrey Sergeevich | Urologist
Education: Diploma in the specialty "Andrology" received after completing residency at the Department of Endoscopic Urology of the Russian Medical Academy of Postgraduate Education in the urological center of the Central Clinical Hospital No. 1 of JSC Russian Railways (2007). Postgraduate studies were completed here by 2010.
Recommended:
Genital Herpes In Men And Women On The Genitals, Treatment Of Genital Herpes

Genital herpes in men and women on the genitalsContent:What is genital herpes?Signs and symptomsCauses of genital herpesWhy is genital herpes dangerous?Sex with genital herpesTreating genital herpesGenital herpes during pregnancyPrevention of genital herpesWhat is genital herpes?
Itching In The Anus In Women And Men - Causes And Treatment

Itching in the anus in women and menItching in the anus is quite painful. The feeling of severe discomfort makes a person scratch the anus, which is often accompanied by injuries. The problem of anal itching is quite delicate, but since it can touch any person, regardless of gender and age, it must be discussed and solved
Diffuse Changes In The Renal Parenchyma - Cyst Of The Renal Parenchyma, Thinning Of The Parenchyma

Renal parenchyma changesDiffuse changes in the renal parenchymaThe kidney is covered with a connective capsule, which consists of a specific tissue, urine excretion and storage system. Specific tissue is a group of cells consisting of the medulla and cortex
Renal Failure - Treatment Of Renal Failure With Folk Remedies And Methods

Treatment of renal failure with folk remediesRenal failure in remission, without symptoms of exacerbation, is usually treated on an outpatient basis. The treatment process is accompanied by control by a urologist, nephrologist, correction of doctor's prescriptions depending on the patient's condition and laboratory tests
Treatment Of Chlamydia In Women And Men - Treatment Regimen

Chlamydia treatment regimen in women and menChlamydia is a sexually transmitted disease that in most cases manifests itself unpredictably. The complexity of its treatment lies in the fact that even after undergoing a course of antimicrobial therapy, the patient is not insured against the exit of the infection from the latent period and the resumption of the clinical picture of the disease