2024 Author: Josephine Shorter | [email protected]. Last modified: 2024-01-07 17:49
Causes, symptoms and treatment of angioedema
Content:
- What is Quincke's edema?
- Quincke's edema symptoms
- Causes of Quincke's edema
- Urgent care
- Treatment of angioedema
- Diet with angioedema
What is Quincke's edema?
Quincke's edema is a local edema (diffuse or limited) of mucous membranes and subcutaneous tissue, which suddenly appears and develops rapidly. A German doctor, a therapist and surgeon by profession, Heinrich Quincke, after whom pathology is named, first discovered and described its symptoms in 1882. Quincke's edema can also be called angioedema (or angioedema), giant urticaria. Giant urticaria is observed mainly in young people, while in women it is more common than in men. According to statistics, the prevalence of this disorder in children has been increasing recently.
Giant urticaria is a common allergy. But in this case, the vascular component is more pronounced. The development of the reaction begins with the antigen-antibody stage. Allergy mediators affect blood vessels and nerve trunks, cause disruption of their work. There is an expansion of blood vessels, an increase in their permeability. As a result, plasma penetrates into the intercellular space and local edema develops. Disruption of the work of nerve cells leads to paralysis of the nerve trunks. Their depressive effect on blood vessels ceases. In other words, the vessels do not come into tone, which in turn contributes to an even greater relaxation of the vascular walls.
Most patients have a combination of edema and acute urticaria.
Quincke's edema symptoms

Quincke's edema is characterized by a sharp onset and rapid development (over several minutes, less often hours).
Quincke's edema develops on organs and parts of the body with a developed layer of subcutaneous fat and is manifested by the following symptoms:
- Swelling of the respiratory system, more often the larynx. With edema of the larynx, hoarseness appears, breathing becomes difficult, accompanied by a barking cough. There is also a general anxiety in the patient. The skin on the face first becomes blue, then pale. Sometimes pathology is accompanied by loss of consciousness.
- Local edema of various parts of the face (lips, eyelids, cheeks).
- Edema of the oral mucosa - tonsils, soft palate, tongue.
- Swelling of the genitourinary tract. It is accompanied by signs of acute cystitis and acute urinary retention.
- Cerebral edema. It is characterized by neurological disorders of various kinds. These can be various convulsive syndromes.
- Edema of the digestive tract. It is characterized by signs of an "acute" abdomen. Possible dyspeptic disorders, acute abdominal pain, increased peristalsis. Manifestations of peritonitis may be observed.
Often, angioedema spreads to the lower lip and tongue, larynx, which leads to a deterioration in respiratory function (otherwise asphyxia). Edema on the face also threatens to spread the process to the lining of the brain. In the absence of emergency assistance from qualified specialists, in this case, a lethal outcome is possible.
Causes of Quincke's edema

The causes of Quincke's edema can be different:
-
The consequence of an allergic reaction that occurs upon contact with an allergen.
The most common allergens are:
- certain foods (fish, citrus fruits, chocolate, nuts)
- preservatives and colors found in food (often in sausages, hot dogs, cheeses)
- pollen
- down, bird feathers and animal hair
- poison or insect saliva that enters the human body through insect bites (wasps, bees, mosquitoes, mosquitoes, etc.)
- household dust
- Consequence of a parasitic or viral infection (giardiasis, helminthic infestations, hepatitis).
- Edema of non-allergic origin (pseudo-allergic reactions), reflecting another somatic pathology, for example, functional disorders of the digestive system.
- A tendency to edema can manifest itself in people with disorders of the endocrine system, including the thyroid gland.
- Edema provoked by tumor and blood diseases.
- Edema arising under the influence of chemical (including medicines) and physical (pressure, temperature, vibration) factors. Drug allergy most often occurs on drugs of the class of analgesics, sulfa drugs, antibiotics of the penicillin group, less often - cephalosporins.
-
Hereditary angioedema resulting from a congenital disorder - deficiency of certain enzymes (C-1 inhibitors of the complementary system), which are directly involved in the destruction of substances that provoke tissue edema. This pathology is more typical for men, it is provoked by injuries, excessive stress on the nervous system (for example, stress), an acute illness.
30% of cases of Quincke's edema are diagnosed as idiopathic, when it is not possible to determine the root cause of the disease.
Emergency care for Quincke's edema

Quincke's edema develops very unpredictably and poses a threat to the patient's life. Therefore, the first thing to do is call an ambulance, even if the condition is currently satisfactory and stable. And in no case should you give in to panic. All actions must be quick and clear.
Before the arrival of the emergency ambulance team
- It is necessary to seat the patient in a comfortable position, to calm down
- Limit contact with the allergen. When bitten by an insect (wasp, bee), remove the sting. If you cannot do this on your own, you need to wait for the arrival of specialists.
- Give an antihistamine (fencarol, diazolin, diphenhydramine). Injectable forms of antihistamines are more effective, since it is possible that edema of the gastrointestinal tract develops and the absorption of substances is impaired. In any case, it is necessary to take 1 - 2 tablets of the drug if it is not possible to give an injection. The medicine will ease the reaction and ease the condition before the ambulance arrives.
- Be sure to drink plenty of alkaline drinks (for 1000 ml of water, 1 g of soda, or narzan, or Borjomi). Drinking plenty of fluids helps to remove the allergen from the body.
- Enterosgel or ordinary activated carbon can be used as sorbents.
- In order to reduce swelling and itching, a cold compress, a heating pad with cold water, ice can be applied to the edematous area.
- Provide good access to fresh air, remove objects that obstruct breathing.
With a severe degree of edema, it is better not to take any measures on your own so as not to provoke a deterioration in the patient's condition, and wait for an ambulance. The main thing is not to harm.
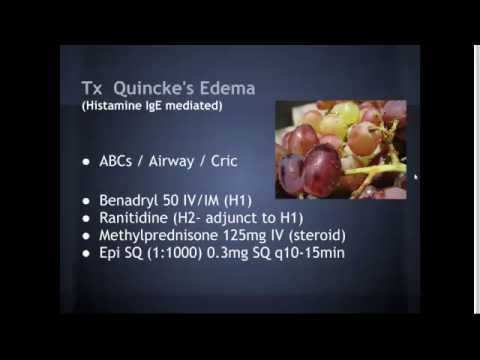
After the arrival of an emergency ambulance
The provision of emergency care is aimed at the implementation of several tasks.
Termination of exposure to the body of the alleged allergen. Necessary to avoid progression of the disease. A cold compress has a good effect. A hot water bottle with cold water or ice will do. If the swelling is the result of an insect bite or medication injection, a tourniquet should be applied above the bite / injection site for 30 minutes.
Hormone therapy. Glucocorticosteroid therapy is necessary to eliminate edema and normalize respiratory function. For giant urticaria, prednisone is the drug of choice. When Quincke's edema is combined with urticaria, dexamethasone can be used.
Desensitizing therapy. Antihistamines are used to reduce the body's sensitivity to repeated exposure to allergens. Suprastin, diphenhydramine, tavegil or pipolfen are injected intramuscularly.
On the subject: All information about allergies
Symptomatic therapy
Saline and colloidal solutions are administered in order to prevent a decrease in pressure and normalize the volume of circulating blood. Most often they use 500-1000 ml of saline, 500 ml of hydroxyethylated starch, 400 ml of polyglucin. After the volume of circulating blood reaches normal values, vasopressor amines can be used: norepinephrine in a dose of 0.2 - 2 ml per 500 ml of glucose 5%; dopamine at a dose of 400 mg per 500 ml of glucose 5%. The dose of drugs is adjusted until a systolic pressure of 90 mm Hg is reached. Art.
For bradycardia, subcutaneous injections of atropine (0.3-0.5 mg) are recommended. If necessary, atropine is administered every 10 minutes.
If bronchospasm develops, agonists and other bronchodilator and anti-inflammatory drugs are used through a nebulizer.
Cyanosis, dry wheezing, dyspnea are indications for the use of oxygen therapy.
In rare cases, catecholamines such as ephedrine and adrenaline may be used.
Anti-shock therapy
For anaphylactic shock, epinephrine is administered. The injection can be repeated if necessary. The break between injections should be at least 20 minutes. With unstable dynamics and the likelihood of death, intravenous administration of epinephrine is allowed. (1 ml of 0.1% epinephrine per 100 ml of saline). In parallel with the introduction of epinephrine, blood pressure, heart rate, respiration are monitored. In adults, blood pressure should not fall below 100 mm Hg. Art. For children, this figure is 50 mm Hg. Art.
With anaphylactic shock during the provision of an ambulance, several rules are required:
- the patient must lie
- the head should be lower than the legs and turned to the side
- the lower jaw should be extended, removable dentures removed from the oral cavity
Treatment of angioedema

Therapeutic measures for angioedema are carried out in two stages: stopping the acute process, eliminating the causes of the disease. After providing an ambulance, the patient is sent to the inpatient department. The choice of department is determined by the nature and severity of angioedema. In severe anaphylactic shock, the patient is admitted to the intensive care unit; in case of laryngeal edema, this can be both resuscitation and ENT department. The onset of abdominal syndrome is a direct indication for hospitalization in the surgical department. If the angioedema is of moderate severity and there is no threat to the patient's life, he can be referred to the allergy or therapeutic department.
Treatment for recurrent giant urticaria (stage 2) depends on the type of disease.
Complete limitation of the patient's contact with the identified allergen is a prerequisite for the successful treatment of giant urticaria, which develops according to the principles of a true allergic reaction. This is of paramount importance in case of edema, which is a consequence of allergy to one or another allergen (food, dust, wool, insect bite, medications, etc.). If the allergen is of a physical nature, it is also necessary to eliminate its pathological effect on the patient (use photoprotective creams for edema caused by exposure to light, refuse to use chilled drinks and foods for edema caused by cold, etc.).
Treatment for worsening giant urticaria is with antiallergic medications. As antagonists of histamine H1 receptors, fexofenadine, loratadine, desloratadine, acrivastine, cetirizine are used. These are new generation antihistamines that have fewer side effects compared to 1st generation antihistamines. Do not cause dryness of mucous membranes, bronchospasm, in therapeutic doses do not affect the cardiovascular system. Low positive dynamics in the appointment of H1 receptor antagonists requires additional prescription of H2 receptor antagonists (ranitidine, famotidine, cimetidine). Treatment can also be carried out with calcium channel blockers (20-60 mg per day of nifedipine) and leukotriene receptor antagonists (10 mg per day for montelukast).
Treatment of angioedema of non-allergic origin is carried out after aggravated detailed clinical examination and identification of the true cause of the disease. The defining stage is the treatment of the identified somatic pathology (treatment of parasitic invasion, therapeutic and prophylactic measures to improve the body and eliminate foci of chronic infection, such as tonsillitis, treatment of endocrine pathologies, therapy of diseases of the digestive system, etc.). Patients are shown a diet with limited consumption of foods containing large amounts of histamine, tyranim.
In case of edema associated with systemic disorders of the connective tissue, it is advisable to prescribe colchicine, sulfasalazine and other drugs used in rheumatology.
In the treatment of hereditary angioedema, there are significant, fundamental differences from treatment with standard therapeutic regimens. Unrecognized hereditary edema in a timely manner and its incorrect treatment in most cases leads to death.
Treatment of hereditary angioedema in the acute phase is aimed at replacing the C-1 inhibitor and compensating for its deficiency. Plasma (fresh or frozen) is most often used for this purpose. In addition, tranexamic acid or aminocaproic acid is administered intravenously. You can also enter danazol at a dose of 800 mg per day or stanozolol at a dose of 12 mg per day. Edema localized to the face and neck requires the administration of dexamethasone and diuretics.
Medicines used for angioedema
- The first generation of drugs: chloropyramine (suprastin), promethazine (pipolfen, diprazine), fencarol (hifenadine), pheniramine (avil), dimethindene (fenistil), tavegil (clemastine), mebhydrolin (omeril, diazolin) act quickly (after 15-20 minutes). They are effective in relieving angioedema, but cause drowsiness, lengthen the reaction time (contraindicated for drivers). They act on H-1 histamine receptors.
- The second generation blocks histamine receptors and stabilizes mast cells, from which histamine is released into the bloodstream. Ketotifen (zaditen) effectively relieves airway spasms. It is indicated for a combination of angioedema with bronchial asma or broncho-obstructive diseases.
- Third-generation antihistamines do not depress the central nervous system, block histamine receptors and stabilize the mast cell wall: Loratadin (Clarisens, Claritin), Astemizole (Astelong, Hasmanal, Isalong), Semprex (Acrivastin), Terfenaddin (Teridin, Trexil), Allerastingodil (Acelastingodil) Zyrtec, Tsetrin (cetirizine), Telfast (fexofenadine).
On the subject: Antihistamines of the 1st, 2nd and 3rd generations - the pros and cons
Prednisone for Quincke's edema

Prednisolone - a systemic glucocorticoid, is used to provide emergency care for angioedema, has anti-edema, anti-inflammatory and antihistamine effects. The antiallergic action of prednisone is based on several effects:
- Immunosuppressive effect (decreased antibody production, inhibition of cell growth and differentiation).
- Prevention of mast cell degranulation
- Direct inhibition of secretion and synthesis of mediators of an allergic reaction
- Decrease in vascular permeability, due to which edema decreases, pressure rises, and bronchial permeability improves.
With angioedema, prednisolone is administered intravenously at a dose of 60 - 150 mg. For children, the dosage is calculated depending on body weight: 2 mg per 1 kg of body weight.
The use of prednisolone can cause agitation, arrhythmia, arterial hypertension, ulcer bleeding. These are the main side effects of systemic glucocorticoids. Therefore, severe hypertension, peptic ulcer disease, renal failure, hypersensitivity to glucocorticosteroids are direct contraindications to the use of prednisolone.
Diet with angioedema

Diet therapy is an integral part of the treatment of any disease. It is very important to take into account the pathogenetic mechanisms of the disease, the state of various organs and organ systems when developing a dietary diet. In the case of treatment of Quincke's edema, a properly selected diet is especially important, because the edema is of an allergic nature.
A diet for Quincke's edema is developed taking into account several fundamental principles:
- When developing a dietary menu for a patient with angioedema, it is necessary to be guided by the principle of elimination. In other words, it is necessary to exclude from the patient's menu foods that can cause a direct or cross-allergic reaction. The dietary menu should not contain foods high in amines, including histamine, foods with high sensitizing properties. Products should, if possible, be natural and not contain synthetic food additives.
- The nutritious diet must be carefully thought out, the products excluded from it must be correctly replaced. This will allow you to optimally adjust the qualitative and quantitative composition of the menu.
- The third principle is the principle of "functionality". Products should be beneficial, help maintain and promote health.
If you follow the advice and rules of nutritional therapy, positive dynamics will be observed. However, diet therapy becomes the most necessary, relevant and effective measure in those cases when a certain food product acts as an allergen.
Exclusion from the diet of foods - allergens is based on data from patient examinations, information about food intolerance. You can simplify the task by keeping a food diary. The determination of allergen products is carried out by various methods, including an open elimination-provocative test, the determination of specific antibodies to food proteins, provocative sublingual tests, and skin tests. Fish and seafood, chicken, eggs, nuts, honey, citrus fruits - those products that most often act as provocateurs of the development of allergic reactions and edema.
If everything is clear with products that cause direct allergic reactions and methods of their identification, then with the identification of an allergic reaction to food of a non-immune nature (otherwise, pseudo-allergic reactions to food), the situation is more complicated. It is more difficult to differentiate such reactions. They are usually determined by the dependence of the development of the reaction on the "dose" of the allergen. If in case of "true" allergic reactions the consumption of the allergen is completely excluded for a long time, then in the case of a pseudo-allergic reaction its inclusion in the diet is acceptable. The amount of allergen product is selected individually for each patient. When developing therapeutic nutrition, the possibility of cross-allergy between all kinds of allergens cannot be excluded.
The most common foods that can cause "true" and pseudo-allergic reactions are:
- Fish and seafood, chicken and eggs, soy, milk, cocoa, peanuts often cause true allergic reactions. Of plant foods, the most allergens are tomato, spinach, bananas, grapes and strawberries.
- Pseudo-allergic reactions can be caused by the same foods as true allergies. You can add chocolate, spices, pineapple to the list.
- Care should be taken to include foods containing biogenic amines and histamine in the menu. These are fish (cod, herring, tuna) and shellfish, cheese, eggs, spinach, rhubarb, tomatoes, sauerkraut. People with allergies should avoid wine.
- You need to exclude from the menu products that contain nitrogen-containing extractive compounds. These are legumes (lentils, beans, peas), black tea, coffee and cocoa, broths, stews and fried meat and fish dishes.
Synthetic food additives often cause allergies and edema. Among them are preservatives (sulfites, nitrites, benzoic acid and its derivatives, etc.) and dyes (tartrazine, amaranth, azorubin, erythrosine, etc.), flavorings (menthol, vanilla, cloves and cinnamon, glutamates) and taste stabilizers.
RELATED: List of Most Popular Food Allergens in Adults
The most common food and substance combinations that can cause cross-allergy are:

- Nuts can provoke allergies not constantly, but during the flowering period of hazel
- Apples increase the risk of an allergic reaction when combined with pears, cherries, cherries, and quince.
- Certain products often provoke allergic reactions when used simultaneously with certain medications. So, you cannot combine the intake of acetylsalicylic acid with the consumption of berries and fruits (grapes, raspberries, strawberries, peaches, apricots and plums). A chicken egg gives a reaction while taking interferon and lysozyme. Kefir should not be consumed during treatment with penicillin antibiotics.
- Bread and cereal dishes are not in themselves allergens. And at the same time, they can cause a reaction during the flowering of cereal plants (wheat, rye, oats, wheatgrass).
- It is undesirable to consume kefir simultaneously with molds, moldy varieties of cheeses.
- Cow's milk can become an allergen if consumed simultaneously with veal and beef foods and dishes. It is undesirable to drink cow and goat milk at the same time.
- When consuming seafood and fish, you should opt for one thing. The simultaneous consumption of fish dishes with shrimp, shellfish, crabs or caviar can also lead to allergies.
Thus, for the prevention and treatment of Quincke's edema, it is very important to correctly formulate the patient's nutritional diet, completely or partially excluding eggs, fish dishes, chocolate, nuts, citrus fruits from the menu. These foods can cause angioedema, even if they are not the root cause of the allergy. In this way, the risk of developing edema can be minimized.
Quincke's edema is a dangerous disease that poses a threat not only to health, but also to human life. It should be treated responsibly. These patients can be advised the following. First, always have an anti-allergic drug on hand. Secondly, try to completely eliminate contact with the allergen. Thirdly, always have a bracelet or an individual card with you indicating your full name, date of birth, contact phone number of the attending physician. In this case, with the sudden rapid development of the disease, even strangers who find themselves next to the sick person will be able to orient themselves and provide timely assistance.

The author of the article: Kuzmina Vera Valerievna | Endocrinologist, nutritionist
Education: Diploma of the Russian State Medical University named after NI Pirogov with a degree in General Medicine (2004). Residency at Moscow State University of Medicine and Dentistry, diploma in Endocrinology (2006).
Recommended:
The First Symptoms Of A Stroke And 7 Emergency First Aid Measures

The first symptoms of a stroke and 7 emergency first aid measuresOften times, healthcare professionals are in the wrong place at the wrong time. And when they appear, they begin to notice how many people have smoked cigarettes or how many of them are in the ashtray, as well as the amount of alcohol drunk or randomly taken or scattered medicines
First Medical And First Aid For Stroke

First medical and first aid for strokeThe criteria for the need for medical care if a stroke is suspected may be the signs shown in the table: For hemorrhagic stroke (cerebral hemorrhage) With ischemic stroke (brain cell death) Severe headache;Sudden, violent vomiting without nausea;Decreased hearing and vision;Half body paralysis;Salivation;Distortion of facial expressions;Clouding of consciousness or its complete loss; The gradual de
Dislocation Of Fingers And Toes - Symptoms, First Aid And Treatment

Dislocation of fingers and toesThe sudden and violent contraction of the muscles causes dislocation of the fingers and toes. Such an injury consists in the displacement of the articular surfaces of the bones. Dislocations of the fingers are quite painful, since there are a large number of nerve endings in the hand
Dislocated Ankle - Symptoms, First Aid And Treatment

Dislocated ankleAnkle dislocation is a fairly common injury to the lower extremities. The risk group includes retirees, athletes, and women who prefer to wear high-heeled shoes. Doctors note that people most often turn to this problem during the cold season, when it is icy outside
Rib Fracture - Signs And Symptoms, First Aid For Rib Fracture. Classification And Treatment

Broken ribsSigns, symptoms, classification and treatment of rib fractureWhat is a fractured rib?Broken ribs are the most common chest injury. Of the total number of fractures, about 16% are rib fractures. In people of a rather advanced age or with certain chronic diseases, rib injuries are much more common, since the elasticity of important bone structures of the chest decreases with age