Pancreatic cancer causes, symptoms and treatment
What is Pancreatic Cancer?

Pancreatic cancer is one of the malignant neoplasms of the pancreas, which is a tumor growth of atypical cells of the glandular or squamous epithelium lining the acinar elements or ductal system. Despite the achievements of modern medicine in the diagnosis and treatment of oncological diseases, pancreatic cancer continues to be one of the unsolved problems of oncology. This is due to the peculiarities of the anatomical location of the organ in combination with the rather rapid development and progression of its tumor transformation.
According to statistics from various sources, the prevalence of pancreatic cancer is from 9 to 11 cases per 100 thousand population. Mostly people of middle and older age are ill: from 40 to 75 years. There are cases of the disease at a younger and older age. The male population is sick almost twice as often as the female. Pancreatic cancer is much more common in developed countries of Europe, North America, Russia, Canada than in African, South American and Asian countries.
The frequency of lesions by the oncological process in different parts of the pancreas is not the same. In more than 90% of cases, tumors with localization in the head of the organ are diagnosed. The remaining 10% is evenly distributed between the body and tail of the pancreas. As for specific types of cancer, they depend on the primary cellular substrate of the tumor and can be as follows:
- Ductal adenocarcinoma (incidence from 75% to 90%);
- Giant cell adenocarcinoma (prevalence is about 6%);
- Glandular squamous cell carcinoma (recorded in 3-4% of patients);
- Mucinous adenocarcinoma (incidence 1-3%);
- Rare types of cancerous tumors of pancreatic tissues: insuloma, glucagonoma, gastrinoma (occupy no more than 1% in the general statistics).
Most cases of pancreatic cancer, regardless of the histological type and location of the tumor focus, are diagnosed when they reach a size of 4-5 cm. And such parameters are characterized by a violation of the structure of the organ, germination of important anatomical formations, regional and distant metastasis!
How long do people with pancreatic cancer live?
The disease belongs to the category of the most serious pathology, since it is quite difficult to diagnose in the early stages of development. Operative technologies and chemotherapy carried out according to a radical oncological treatment program are not always well tolerated by patients due to the trauma and aggressiveness towards the body. The combination of all these factors minimizes the patient's chances of survival. The median (mean) life expectancy among people with established pancreatic cancer is 6 months to a year. No more than 1-5% of patients manage to survive the five-year line.
The disease detected in the early stages has a slightly more favorable prognosis, but they depend little on the timeliness of the treatment. The operation, due to its great complexity, often ends in death in the early or late postoperative period.
On the subject: Selenium reduces the risk of cancer by 2 times!
Such disappointing data raise pancreatic cancer into a special category of oncological diseases. No other type of cancer has such sad statistics. In recent years, there has been a tendency towards an increase in the incidence rate while maintaining poor indicators of early diagnosis. In 85-90% of cases, the disease is found in the late stages, when a cure becomes impossible. Earlier diagnosis of the disease is hampered by the long asymptomatic course of cancer and its deep location with retroperitoneal localization, which makes it invisible even for the most modern research methods. Early detection of pancreatic cancer is often an accidental finding when performing diagnostic procedures for other diseases.
Content:
- Pancreatic cancer symptoms
- Pancreatic Cancer Causes
- Pancreatic cancer grades
- Pancreatic Cancer Diagnosis
- Pancreatic cancer with metastases
- Pancreatic cancer treatment
- Pancreatic cancer nutrition
Pancreatic cancer symptoms

Despite the poor statistical indicators of pancreatic cancer, in no case should we give up the fight against it. After all, such a path will definitely be a dead end. Early diagnosis of the disease can help the sick person get into the 1-5% of patients with a five-year survival rate. After all, there are cases of life expectancy after an established diagnosis of pancreatic cancer and more than ten years.
Therefore, it is unacceptable to despair. The usual alertness, which should not be manic, combined with an attentive attitude to all changes in the body, will help to identify the disease in the early stages and take active measures to combat it.
Symptoms of pancreatic cancer include:
- Epigastric and deep pain in the lower back and left hypochondrium. It can have different intensities. Its appearance marks the progression of the disease. The dependence is directly proportional: the more intense the pain syndrome, the more difficult the stage of the pathological process;
- Loss of appetite. It occurs practically from the first stages of the disease and gradually increases;
- Symptoms of diabetes mellitus are thirst, persistent dry mouth, polyuria (an increase in the amount of daily urine). The manifestation of pancreatic cancer in 15% of cases occurs precisely from such symptoms;
- Frequent thrombophlebitis of the lower extremities. Sometimes the first manifestation of pancreatic cancer is persistent or recurrent inflammation of the superficial veins of the lower extremities for no apparent reason (absence of varicose veins, injuries or other risk factors for the development of vascular pathology);
- Enlargement of the abdomen. It rarely acts as the first sign of the disease, but in advanced cases it always occurs. The appearance of such a symptom is associated with metastatic lesions of the peritoneum (carcinomatosis) and the accumulation of ascitic fluid in the abdominal cavity.
The first signs of pancreatic cancer
Early signs include:
- Bloating and discomfort in the stomach (epigastric region). Refers to the earliest signs of the disease, observed in more than 30% of patients;
- Malaise and unmotivated general weakness is another early symptom of the disease in 25% of cases;
- Weight loss for no apparent reason. 98% of patients note this symptom;
- Nausea with intermittent vomiting and other digestive disorders. This symptom is observed in 45-50% of cases;
- Yellowness of the skin. One of the most frequent and only signs of the disease (in 65% of cases) with the localization of the tumor process in the head of the organ. Jaundice is mechanical in nature, and occurs as a result of compression of the common bile duct, which passes through the thickness of the pancreatic tissue. Yellowing of the skin can appear even with a small tumor, while it still does not go beyond the organ. But in most cases, the presence of the first symptoms of the disease in the form of jaundice characterizes severe forms of cancer;
Pancreatic Cancer Causes

Speaking about pancreatic cancer in general, we can say that it is a polyetiological disease. Many differently directed factors can act as its causes. Whatever they turn out to be, the consequences of the pathological influence on the tissues of the pancreas end in the defeat of cellular DNA. As a result, there is a mutation of the genes of epithelial, glandular, or endocrine cells responsible for triggering their apoptosis (programmed death). Ultimately, cells acquire abnormal properties, become completely different from healthy ones, lose the ability to perform their functions and begin to divide uncontrollably as long as the body is alive.
Such mutations of genetic cellular material are capable of triggering:
- Chronic pancreatitis. Almost all patients with pancreatic cancer have a history of this disease. The prolonged existence of the inflammatory process is accompanied by the formation of a large number of free radicals and other products of lipid peroxidation. Accumulating in tissues, they can cause damage to the genetic material of the tissues of the pancreas;
- Genetic predisposition and congenital mutations of the p53 and K-ras genes;
- Smoking. The relationship between malignant tobacco smoking and the incidence of cancerous transformation of pancreatic cells has been observed;
- The predominance of meat food in the diet for a long time. This type of nutrition is noted by about 80% of patients;
- Oncogenic viruses. Their role in the initiation of mutations is not precisely established and is under study;
- Chemical and physical carcinogens. They can enter the body from the environment through air, food and water. As a rule, carcinogens are represented by pesticides, herbicides, household chemicals, benzidine derivatives, ionizing radiation and heavy metal salts;
- The influence of alcohol. No direct relationship has been established between pancreatic cancer and alcohol abuse. But if we take into account that alcohol acts as one of the main culprits of chronic pancreatitis, then an indirect effect on the occurrence of cancerous lesions of pancreatic tissues can be considered quite proven.
Interesting fact. Scientists have found that in 95% of patients with pancreatic cancer, Helicobacter Pilori is present in the stomach. So far, only its role in the occurrence of duodenal ulcer has been proven. But many large medical centers continue to conduct research in this direction. It remains to be hoped that experiments will determine the true ability of this pathogen to cause damage to the DNA of pancreatic cells.
See also: Other Cancer Causes and Risk Factors
Pancreatic cancer grades

Staging pancreatic cancer is important. This information is relevant in determining the tactics and treatment plan. Do not confuse the concept of "stage of the oncological process" with the concept of "clinical group" of the disease. If the first reflects the degree of damage and prevalence of the tumor, then the second speaks of the patient's attitude to the treatment. It is more relevant to consider the staging of the process, which is represented by four degrees.
1st degree
From an anatomical and clinical point of view, the first degree of pancreatic cancer should be divided into three types:
- 0 (zero) stage. It is designated by the Latin term carcinoma in situ. It is characterized by the spread of the tumor within the basement membrane of the cell layer from which it develops. Such a tumor does not cause any manifestations and structural rearrangements of the organ, and is not capable of metastasis;
- 1A stage. The tumor invades the basement membrane and reaches 2 cm in size;
- Stage 1B. The size of the tumor exceeds 2 cm, but it has a strictly intraorganic location, does not grow important anatomical structures and does not have metastases.
2nd degree
The basis of the second stage of pancreatic cancer is the exit of the tumor focus outside the organ. The following degrees of the second stage are distinguished:
- 2A - the primary tumor focus is invading vital anatomical structures (choledoch, duodenum, mesenteric vessels, cellulose, ligaments, etc.). In this case, no metastases are recorded;
- 2B - the primary tumor either goes beyond or remains in the thickness of the pancreas, but there are metastases to the extraorgan lymph nodes of the first order.
Grade 3
This stage is based on the metastatic spread of the tumor to regional lymph nodes of the second and third order. In this case, metastases can be recorded in the paraaortic, retroperitoneal, and also lymph nodes along the superior mesenteric, portal, common hepatic arteries and veins. At the same time, the primary tumor itself extends far beyond the organ, invading the stomach, duodenum and blood vessels.
4 degree
The most severe and hopeless form of any cancer, including pancreatic cancer. It is characterized by a wide spread of the primary tumor to all nearby organs, metastasis to all lymphatic collectors. The most important distinguishing feature of stage 4 is metastases in distant organs (liver, lungs, etc.).
Pancreatic Cancer Diagnosis

It is not always easy to suspect and confirm a diagnosis of pancreatic cancer. This is especially true in relation to the early stages of the disease, when the size of the tumor does not exceed 1-2 cm.
For diagnostics are used:
- Ultrasonography. Its conduct involves an examination of all organs of the abdominal cavity and retroperitoneal space. Particular attention is paid to the pancreas. One of the keys to the information content of ultrasound in the diagnosis of cancer is the strict adherence to the rules of preparation. After all, the organ is located deep enough and is difficult to study due to the accumulation of gases in the transverse colon;
- Tomographic research. From this group of diagnostic methods, computed and magnetic resonance imaging (CT and MRI) are used. Preference should be given to the second study, as it better visualizes soft tissue structures, to which the pancreas belongs. The method today has become the gold standard for diagnosing cancer in the early stages. It also allows you to determine the presence of metastases in regional lymph nodes and other organs;
- Blood test for tumor markers. This diagnostic method is based on the immuno-histochemical determination in the blood of the concentration of specific protein molecules and antigens, which are produced by cancerous tumors of the pancreas. These include tumor markers: CA 19-9 and CEA or cancer embryonic antigen. Their standards are set by the specific laboratory conducting the analysis, depending on the reagents used. The rate must be indicated next to the result of the resulting indicator;
- ERCP is an abbreviation for the full name of the method of endoscopic retrograde cholangiopancreatography. This method of diagnosis cannot establish a diagnosis of pancreatic cancer. But it is used to exclude the presence of stones in the bile ducts, which can also cause obstructive jaundice. And it refers to one of the main symptoms of the cancerous process in the head of the organ;
- Pancreatic biopsy. The only reliable way to diagnose cancer can be a histological examination of the pathologically altered area. Performing this diagnostic technique is associated with high risk and technical difficulties. The biopsy is always done under visual control. In this case, the advancement of a thin needle, with which all tissues are sequentially pierced, is monitored under the monitor of a magnetic resonance imager, ultrasound or diagnostic laparoscopic surgery. The last method is the most acceptable.
Pancreatic cancer with metastases
Malignant neoplasms of the pancreas are characterized by early metastasis. This is due to the powerful blood supply to the organ, a large number of lymphatic ducts and lymph nodes.
Therefore, even small tumors, especially highly differentiated adenocarcinomas, are potentially capable of metastasizing along the following pathways:
- Lymphogenous - in the regional lymph nodes along the main arteries, retroperitoneal tissue and liver gates;
- Hematogenous - in the liver, lungs, bones and spine;
- Mixed (a combination of hematogenous, lymphogenous and contact pathways) - in the peritoneum, intestines, stomach and other structures of the abdominal cavity.
Most often, one has to deal with distant metastases to the liver. As a rule, they are constantly progressing in the form of the appearance of new foci, which are constantly increasing in size. At the fourth stage of the disease, the liver of such patients sharply increases in size and takes the form of a tumor conglomerate, consisting of multiple metastatic nodes.
The second most common type of distant metastases is their location in the peritoneum. This condition is called carcinomatosis. Metastases of this type are also prone to a constant increase in size and growth at the site of attachment. In this case, ascites always occurs. Its appearance is explained by irritation of the peritoneum, which responds with an increase in the secretion of intra-abdominal fluid in combination with a violation of its absorption.
The presence of metastases of pancreatic cancer significantly aggravates the course of the disease and dooms the patient to hopelessness in relation to treatment, which under no circumstances will bring good results. Metastases, like the primary tumor, require significant vital resources of the body for its growth. Against this background, the level of protein and hemoglobin in the blood progressively decreases, immunity suffers and severe cancer intoxication occurs with the patient's cachexia.
Find out more: The most effective recipes for restoring the pancreas!
Pancreatic cancer treatment

A comprehensive treatment approach for pancreatic cancer involves:
-
Surgical treatment. Cancer is considered operable 1-2, and in some cases even 3 stages, when the removal of the tumor is technically feasible, and the age and general condition of the patient makes it possible to undergo such a traumatic intervention.
Among the operations performed are:
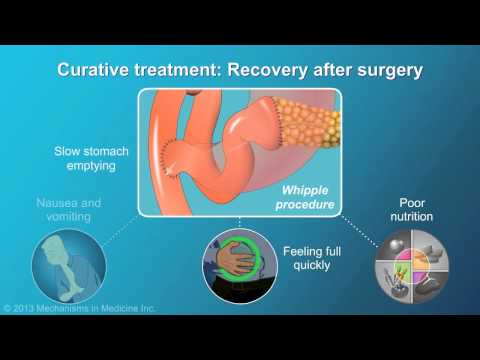
- PDR (classical pancreatoduodenal resection). It is indicated for localization of cancer in the head and areas of the pancreas body close to it. At the same time, lymph node dissection of regional lymphatic collectors is performed. During the operation, the head and body of the pancreas, the duodenum, part of the common bile duct and stomach are removed. After removal of a single block with lymph nodes, the patency of the gastrointestinal tube is restored by anastomosis. The common bile duct and pancreatic duct are sutured to the Roux-off loop of the small intestine. The operation is extremely traumatic, accompanied by a large number of complications and high mortality;
- Pancreas tail resection. Less severe surgery than PDR. It is performed in patients with tumor localization in the tail of the organ. The intervention involves the removal of the distal part of the pancreas along with the spleen and lymph nodes;
- Pancreatectomy and extended resection of the pancreas. The first intervention is performed extremely rarely, and the second may involve PDR or resection of the tail in combination with resection of other organs when they are invaded by a tumor.
- Chemotherapy. It involves the introduction of chemotherapeutic agents that have a toxic effect on tumor cells. The method is often combined with surgical treatment or used as an independent one for inoperable forms of cancer.
- Radiation therapy. In the therapy of pancreatic cancer, it is used extremely rarely. Assumes targeted percutaneous delivery of high doses of ionizing radiation to the tumor;
- Palliative and symptomatic treatment. It includes surgical interventions that restore the patency of the stomach, duodenum and biliary tract. In this case, manipulations with the tumor are not performed. Symptomatic therapy involves the administration of pain relievers and detox medications.
See also: Other treatments
Pancreatic cancer nutrition
The peculiarities of the diet for pancreatic cancer are not given much importance, since the diet does not help much in getting rid of the problem. The only thing that the diet really allows is to avoid an increase in the unpleasant symptoms of digestive disorders, which are often found in this pathology. On the one hand, food should be gentle enough so as not to stimulate the functioning of the altered pancreas with increased pain and signs of enzymatic deficiency. But on the other hand, food must be healthy and nutritious enough to provide the basic necessities of life for the main components.
This balance can be achieved by following the principles outlined in the table:
| Can | It is impossible | |
| Meat and fish dishes | Diet type meat (turkey, rabbit, chicken). Low-fat sea and river fish. They should not be greasy and are steamed. | Meats that are high in fat (pork, beef, duck, goose) and fatty fish. It is unacceptable to use fried, smoked and seasoned dishes. |
| Flour and bakery products | Bread containing bran and wholemeal flour, biscuits and oatmeal cookies. The baked goods should not be very fresh. | Pastries made from rich flour, high sugar content, creams and chocolate (buns, cookies, custard tubes). |
| Milk products | Sour milk, kefir, fermented baked milk, yogurt, low-fat cottage cheese, processed and hard cheese. | Whole fresh milk, fatty sour cream |
| Vegetables and fruits | Any fresh vegetable and fruit salads that do not cause severe bloating and diarrhea. Salads are seasoned with vegetable oils (olive, sea buckthorn, sunflower), yogurt or jam. You can include vegetables in soups and broths, steam. | Sour vegetables and fruits of concentrated ferment. The use of tomatoes and raw cabbage (preferably stewed) is limited. If, against the background of the inclusion of certain foods in the diet, any deterioration occurs, they must be canceled. |
| Cereals | Rice, buckwheat, pearl barley, oatmeal and millet. | Legumes and pea-based dishes |
| Other | Soft-boiled eggs, honey, nuts, a small amount of sunflower oil, fruit drinks, tea, a decoction of dried fruits and compote. | Chocolate, coffee, spices and spices, mushrooms, alcoholic beverages, carbonated water, especially containing dyes. The use of salt and sugar is limited. |
The diet of a patient with pancreatic cancer should be determined by the actual tolerance of specific foods. If the patient has a desire to eat some dish, but it is not included in the list of permitted ones, the person's wishes should be guided. The only thing that must be observed is the rule of gradually introducing products into the diet!
Interesting information: thymokinone, the main active substance contained in black cumin seeds, reduces the size of pancreatic tumors by an average of 67%, and in addition, the level of cytokines in tumors is significantly reduced (powerful anti-inflammatory effect). The studies were conducted on animals with pancreatic cancer at the Kimmel Center (USA).
On the subject: beneficial properties and uses of black cumin oil
An indicative weekly menu for a patient with pancreatic cancer with a five-day diet is presented in the form of a table:
| First meal | Second meal | Third meal | Fourth meal | Fifth meal | |
| Mon. | Kefir and banana | Puree soup, tea with bread and butter | Porridge with boiled cutlet, vegetable salad, compote | Cottage cheese casserole with cocoa | Crackers with yogurt |
| Tue | Milk porridge with butter | Stuffed pepper, herbal tea | Soup with cereals in chicken broth, bread | Fruit and curd casserole, cocoa | Kefir with breadcrumbs |
| Wed | Kefir, oatmeal cookies | Steamed fish cutlets, rice porridge | Beetroot liquid dish (borsch), vegetable salad, compote | Apples baked with jelly | Ryazhenka with biscuit biscuits |
| Wed | Yogurt with biscuit biscuits | Buckwheat porridge with vegetable salad, green tea | Mashed potatoes with a steam cutlet, bread, jelly | Carrot juice, egg omelet | Dried fruit Uzvar with honey |
| Fri. | Baked apple, green tea | Vegetable soup, bran bread | Barley porridge with butter, boiled fish, vegetable salad, compote | Sweet fresh fruit, weak tea | Kefir with breadcrumbs |
| Sat. | Curd casserole, cocoa | Cream soup based on vegetables and rabbit meat | Pasta with butter and doctor's sausage, bread, compote | Milk porridge with fruit jam | A glass of kefir |
| Sun. | Yoghurt with biscuits or breadcrumbs | Creamy soup with potatoes, cauliflower and minced chicken | Fish fillet with boiled vegetables, dried fruit uzvar | Banana with cottage cheese | Yogurt with oatmeal cookies |
On the subject: What foods increase immunity?
This menu is not a standard to be strictly followed. It can be modified in any direction, according to the specific preferences of the sick person. The number of meals can be expanded to 6 or more times a day if the patient is able to eat only small portions.

The author of the article: Bykov Evgeny Pavlovich | Oncologist, surgeon
Education: graduated from residency at the Russian Scientific Oncological Center. N. N. Blokhin "and received a diploma in the specialty" Oncologist"