2024 Author: Josephine Shorter | [email protected]. Last modified: 2023-12-16 21:43
The use of chondroprotectors for spinal hernia
Content:
- Intervertebral disc structure
- How does a hernia develop?
- Chondroprotectors: what is the mechanism of action?
- List of chondroprotective drugs
- Indications for the use of chondroprotectors
- Has the effectiveness of chondroprotectors been proven?
- Reviews on the use of chondroprotectors
Diseases of the spine and joints “get younger” from year to year, and now not only elderly people, but also patients from 30-40 years old, turn to doctors.
Herniated discs, osteochondrosis and joint diseases occur not only due to increased loads and injuries of the musculoskeletal system. The cause of these diseases may be insufficient blood supply to the cartilaginous tissues, which is often found in people with a sedentary lifestyle.
The treatment of intervertebral hernia was previously carried out only with the use of analgesics and non-steroidal anti-inflammatory drugs.
Now, other drugs of conservative treatment have appeared, belonging to the group of chondroprotectors, which not only relieve inflammation, but also contribute to the restoration of cartilage tissue, the volume and viscosity of the articular fluid, while they do not have strong side effects.
Intervertebral disc structure

The intervertebral discs perform the most important function in the body - they provide the strength of the structure of the spine, cushion it when walking and exertion, preventing damage to the spinal cord.
- The intervertebral disc consists of a gelatinous or pulpous nucleus, an annulus fibrosus and two cartilaginous plates.
- The nucleus pulposus has a jelly-like structure and is necessary for cushioning the spine.
- The annulus fibrosus consists of many concentric plates and is fixed on the vertebral body with the help of ligaments. The annulus fibrosus prevents protrusion of the nucleus pulposus, so the formation of a hernia is always associated with its rupture.
- The cartilaginous plates are associated with the vertebral body, annulus fibrosus and nucleus pulposus. When the processes of devascularization begin and the blood supply to the intervertebral discs decreases due to the vessels, further nutrition of the intervertebral discs is provided by the cartilaginous plates.
The height of the intervertebral discs in different parts of the spine is not the same: for example, they are much thicker and tighter to the vertebrae in the cervical and lumbar spine in order to ensure maximum mobility.
A herniated disc in the cervical and lumbar spine is very dangerous, because with the progression of the disease, it can lead to circulatory disorders of the brain or loss of bowel and genitourinary system function.
How does a hernia develop?
A healthy intervertebral disc has a very resilient and elastic annulus fibrosus, with minimal risk of rupture. However, age-related changes in the body, excessive loads and a sedentary lifestyle can provoke degenerative processes in the intervertebral discs, and then the development of the disease becomes quite natural.
Physiological changes in the intervertebral discs lead to a decrease in their elasticity. The annulus fibrosus loses its ability to retain fluid, which threatens dehydration and cracking. In the nucleus pulposus, the amount of collagen increases, while the amount of mucoproteins, on the contrary, decreases. In this state, the intervertebral disc is very vulnerable, there is a risk of rupture of the fibrous ring, which most often occurs in the back of it, where it is least tightly connected to the vertebra. Under the pressure of the nucleus pulposus, the ring first stretches (protrusion), and then breaks. A prolapse or hernia of the intervertebral disc is formed.
Devascularization of the intervertebral discs occurs gradually, further nutrition occurs with the help of cartilaginous plates by diffusion and osmosis. Therefore, there is a need for additional nutrition of the vertebrae, maintaining good blood circulation.
Most of these changes are associated with age, but metabolic disorders, a sedentary lifestyle, and hereditary factors can provoke them.
So, with age, the blood supply to the intervertebral discs decreases due to the blood vessels - this process is called devascularization. Nutrition and a constant blood supply are very important for the health of the intervertebral discs. Violation of blood supply is the reason why a hernia occurs not only in miners and weightlifters, whose spine is under enormous stress, but also in office workers who lead a sedentary lifestyle.
As the load on the spine increases and the misallocation between its sections increases, degenerative processes in the intervertebral discs intensify, which ultimately leads to protrusion of the nucleus pulposus beyond the annulus fibrosus. In the early stages, a hernia may not manifest itself in anything - there is no pain syndrome if the nucleus does not pinch the nerve.
Symptoms of a herniated disc include:
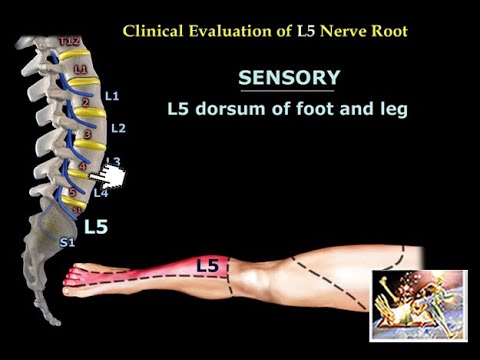
- Pain at the site of hernia localization - if it is located in the lumbar spine, then the pain can be given to the legs and cause numbness. In addition, a hernia of the lumbar spine manifests itself in a number of disorders of the intestines, pelvic organs, reproductive and urinary systems.
- Fatigue and weakness even after little physical activity, such as walking or climbing stairs.
- Partial paralysis or paresis in a certain area of the body is observed with hypertonicity or hypotonia of muscles.
- Sharp pains when trying to bend, stretch the neck or turn the head - pulling syndrome.
- Vertebral artery syndrome - develops with a hernia in the cervical spine and manifests itself as periodic dizziness, headaches, visual and hearing disorders. In the absence of timely treatment, the disease can cause irreversible damage to the central nervous system.
- Radicular syndrome - pain in the area of the affected nerve, weakening and atrophy of muscles in the area of its action, violation of tendon reflexes.
The hernial sac, when protruding, can compress the nerve roots, blood vessels and the spinal cord, which manifests itself with symptoms such as pain and numbness. In the absence of these symptoms, the hernia often remains undiagnosed.
In 10% of hernia cases, patients need surgery. Due to possible complications, it is prescribed only for severe pain, loss of sensitivity of the limbs, loss of control over the urinary system, which leads to spontaneous urination. If a pinched hernia does not have pronounced symptoms, then the doctor prescribes conservative treatment drugs, including chondroprotectors. All types of surgeries to remove herniated discs - indications and consequences
Chondroprotectors: what is the mechanism of action?

The main active ingredients of chondroprotectors - chondroitin sulfate and glucosamine - are structural components of cartilage tissue, without which regeneration of damaged vertebrae and joints is impossible. With their increased concentration in the blood, restoration processes begin in the cartilaginous tissue of the intervertebral discs, pain syndrome and swelling around the damaged area of the spine disappear.
This group of drugs is often characterized as slow-acting symptomatic drugs. With prolonged use, chondroprotectors relieve inflammation and pain, improving the condition of cartilage tissue.
Chondroitin sulfate acts on chondrocytes, stimulates the production of structural components of cartilage, which include collagen, proteoglycan, hyaluronic acid, glycosaminoglycans. It is able to influence the cellular factor of inflammation, reducing its intensity, slows down and stops the destruction of cartilage. Activates the processes of synthesis of intra-articular fluid.
Glucosamine exhibits antioxidant activity, protecting tissues from free radicals, stimulating the production of hyaluronic acid and its own chondroitin, heparin and glycoproteins. Improves the quality of synovial fluid, restoring joint mobility. Reduces the activity of lysosomal enzymes and the number of free radicals.
List of chondroprotective drugs
The active substance of most chondroprotectors is chondroitin sulfate, which is extracted from the cartilaginous tissues of animals.
Experts are discussing which substance in the composition of the chondroprotector is more effective - chondroitin sulfate or glucosamine. In the treatment of arthrosis and hernia of the spine, monopreparations of both one and the other substance are used, so that the final decision remains with the attending physician. Chondroitin has an anti-inflammatory effect, when used externally in the form of an ointment, it can relieve swelling and reduce pain.
Glucosamine stops the processes of destruction of joint tissue, promotes the production of its own chondroitin sulfate and hyaluronic acid.
Modern classification of drugs depending on the composition:
- Monopreparations of chondroitin sulfate: Honsurid, Structum, Chondrolone, Mucosat, Chondroxide, Hondramed;
- Monopreparations of glucosamine: Don, Elbona, Glucosamine sulfate, Farmaskin THC, Aminoartrin;
- Combined drugs: Teraflex, Kondronova, Chondrosamine, Artra.
On the subject: Modern dietary supplements for the restoration of joints
Indications for the use of chondroprotectors
Chondroprotectors are prescribed together with the basic therapy of osteochondrosis and other diseases of the spine, combined with moderate physical activity in the form of exercises to warm up the affected parts, as well as with vitamin therapy under the supervision of a doctor.
Chondroprotectors are taken to reduce painful sensations and inflammatory processes, drugs of this group effectively restore joints in the early stages of arthrosis, promote the regeneration of cartilage tissue and enhance the synthesis of its structural components.
The course of treatment is from six months, and the first qualitative changes will be noticeable only after 2-3 months. Stable improvement occurs after 6 months of use. Therefore, it is recommended to use them for 6-12 months.
The drugs are prescribed internally in the form of a powder or tablets, in the form of an ointment for application in the area of localization of inflammation, as well as intramuscular and intraarticular injections.
Has the effectiveness of chondroprotectors been proven?

Since the cause of the development of a hernia is, first of all, an insufficient supply of nutrients and oxygen to the intervertebral discs, which come from the blood, treatment with chondroprotectors cannot be the only treatment measure. The drugs enter the bloodstream, and together with the blood they must reach the affected area and affect it, but if the blood supply is impaired, the result of such treatment will be zero. Therefore, it is important to perform physiotherapy exercises so that the blood rushes to the muscles and tissues in the area of the hernia, and with it the chondroprotector also flows there.
Herniated disc is the ultimate outcome of intervertebral disc disease. Therefore, chondroprotectors are prescribed not for the treatment of hernia, but in order to restore tissues and prevent degenerative processes in the future.
Clinical trials have shown the effectiveness of chondroprotectors as drugs for the conservative treatment of intervertebral hernia. The course of admission is at least six months or more, with the hernia decreasing by 1 mm every 6 months. Chondroprotectors help prevent the appearance of hernia in other parts of the spine and are an excellent prevention of osteochondrosis.
On the subject: A set of the best exercises for lumbar hernia of the spine
Reviews on the use of chondroprotectors
“I went to the doctor with complaints of pain in the back and legs, and a hernia was found. In addition to anti-inflammatory drugs, the doctor recommended chondroprotectors. After a couple of months of application, pain began to appear less often, the hernia did not disappear anywhere. The doctor said that conservative treatment is ineffective in my case, and chondroprotectors simply reduced pain manifestations."
“I went through a set of procedures for the treatment of hernia in the clinic. The doctor prescribed Chondroxide in combination with iontophoresis, plus physiotherapy exercises. Pain sensations disappeared already in the second month after the procedures, but not completely, sometimes pains appear. The hernia did not go away, but no new pinches were found."
“I took Teraflex a capsule a day for pain in joints and lower back. The back stopped bothering by the end of the first week of admission, but the knees hurt from time to time, although not as much as before. The doctors did not find hernia and prolapse"
“At one time I tried many popular chondroprotectors to relieve pain from lumbar hernia. I took Don in capsules, applied Chondroxide in the form of an ointment externally - ineffectively. It helped only in combination with phonophoresis, the pains disappeared, the hernia slightly decreased, but did not disappear completely."

Author of the article: Kaplan Alexander Sergeevich | Orthopedist
Education: diploma in the specialty "General Medicine" received in 2009 at the Medical Academy. I. M. Sechenov. In 2012 completed postgraduate studies in Traumatology and Orthopedics at the City Clinical Hospital named after Botkin at the Department of Traumatology, Orthopedics and Disaster Surgery.
Recommended:
Flashing Flies Before Your Eyes - Where Are They From? Are They Dangerous? Treatment Methods

Flashing flies before your eyes: causes and treatmentFlies flash before people's eyes for a reason. This phenomenon is an ophthalmic symptom in which polymorphic opacities are observed in the visual field. Flies can have different colors and shapes, they can look like elongated threads, small grains, rings, cobwebs
Foot Fungus - Symptoms, Effective Treatment Of Foot Fungus, A List Of Inexpensive Drugs

Causes, symptoms and treatment of foot fungusWhat is foot fungus?Foot fungus is a mycotic lesion of the skin of the interdigital spaces with the possibility of including toenails in the pathological process (onychomycosis) and further spreading to other parts of the human body
Relief Candles - Are They Effective? Instructions For Use, Types Of Candles, Composition, Analogues

Relief candles - instructions for useRelief is a drug that is aimed at treating hemorrhoids and relieving a person from anal itching. With it, you can get rid of eczema and anal fissures. The drug is available in the form of suppositories and in the form of an ointment
Antihypoxants - What Are They? List Of Drugs

List of antihypoxants for hypoxiaMost hospital patients undergoing therapy for various chronic pathologies note that in addition to the main treatment, they are often prescribed antihypoxants and antioxidants. Also, after discharge from the hospital, doctors strongly recommend taking a course of vitamins that have an antioxidant effect
Epilepsy Treatment - A List Of Effective Remedies And Drugs

Epilepsy treatmentContent:Omega-3 reduces seizures by 33%Treatment of epilepsy with folk remediesDrink 1000 Skvortsova A.V.Medical treatment for epilepsyRemoval of status epilepticusSurgical treatment of epilepsyEpilepsy is a chronic disease that affects the patient's brain and is accompanied by a predisposition to seizures with loss of consciousness